Unrealistic Expectations, Eating Disorders, and Mental Health
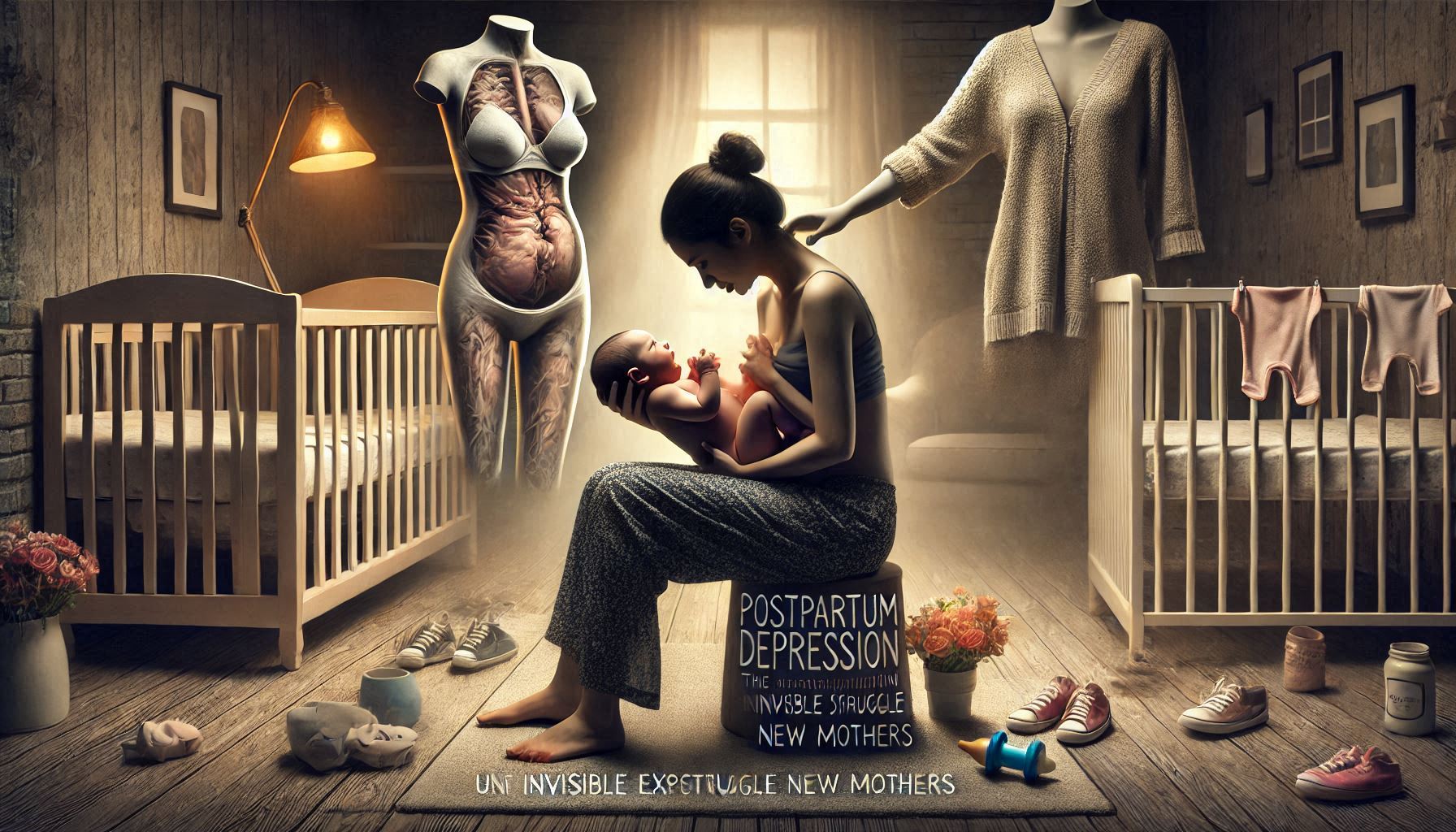
The birth of a child is often romanticized as a beautiful and joyful occasion, where a new mother experiences instant love and bonding with her baby. While this narrative holds true for many, the reality for countless other new mothers is far different. For a significant number of women, the period following childbirth is marked by overwhelming emotional distress, feelings of sadness, and a deep sense of isolation. This condition, known as postpartum depression (PPD), is one of the most common and debilitating mental health challenges faced by women after childbirth. However, despite its prevalence, postpartum depression remains largely underreported and misunderstood.
In this guide, we will explore the complexities of postpartum depression, examining how unrealistic societal expectations, body image pressures, and eating disorders intersect to exacerbate the emotional and psychological burden of new mothers. We will also look into how society, healthcare systems, and support networks can better support mothers during this vulnerable time. Our goal is to shed light on the invisible struggle many new mothers face and to advocate for a more compassionate and supportive approach to maternal mental health.
Understanding Postpartum Depression: More than Just “Baby Blues”
What is Postpartum Depression?
Postpartum depression is a serious mental health condition that affects an estimated 1 in 7 women after childbirth. It is characterized by persistent feelings of sadness, anxiety, irritability, and exhaustion that interfere with a mother’s ability to care for herself or her baby. Unlike the “baby blues,” which affect many women for a few days or weeks after childbirth, postpartum depression can last for months or even longer if untreated.
The symptoms of postpartum depression are far more severe than the transient emotional ups and downs that many mothers experience in the immediate aftermath of birth. Women with PPD may experience:
- Emotional numbness or a complete lack of joy in activities that once brought happiness.
- Irritability and anger toward their baby, their partner, or themselves.
- Severe fatigue and difficulty sleeping, even when the baby is asleep.
- Feelings of hopelessness and worthlessness, sometimes leading to thoughts of harming themselves or the baby.
- Difficulty bonding with the baby, which can make caring for the child emotionally and physically exhausting.
While the exact cause of postpartum depression is not entirely understood, a combination of hormonal changes, psychological stress, and environmental factors is believed to contribute to its development. During pregnancy, women undergo dramatic hormonal shifts, and after childbirth, these hormone levels drop rapidly, which may contribute to feelings of sadness and depression. Additionally, factors like a lack of sleep, breastfeeding challenges, and the emotional and physical demands of motherhood can further exacerbate these feelings.
The Stigma and Underreporting of PPD
Despite its prevalence, postpartum depression remains underreported and underrecognized. One of the reasons for this is the stigma surrounding mental health and motherhood. Society often perpetuates an idealized version of motherhood that portrays it as a naturally joyful and fulfilling experience. Mothers are often expected to bond with their babies instantly and to thrive in the role of caregiver. These unrealistic expectations can make it difficult for mothers to admit that they are struggling emotionally.
In addition, women may fear being judged for not feeling “happy” after childbirth. There is often an unspoken pressure to “bounce back” quickly, both emotionally and physically, after giving birth. This societal pressure can leave women feeling isolated, ashamed, and reluctant to seek help. Consequently, many mothers silently suffer, fearing that their struggles will reflect poorly on their abilities as parents.
The Impact of Postpartum Depression on Families
Postpartum depression not only affects the mother but can also have profound effects on the family dynamic. The emotional toll of PPD can strain relationships with partners, family members, and even the baby. Partners may feel helpless or frustrated if they don’t understand the severity of the situation, leading to communication breakdowns or feelings of alienation. In severe cases, a mother’s inability to bond with her baby due to PPD can result in attachment issues that may affect the child’s emotional development.
It is essential to recognize that PPD is a medical condition, not a personal failing. When left untreated, postpartum depression can lead to long-term consequences for both the mother and the child. Early intervention is crucial in managing symptoms and supporting mothers in their recovery.
Unrealistic Expectations of Motherhood
The Myth of the Perfect Mother
The modern portrayal of motherhood, particularly in the media and on social media platforms, creates an unrealistic image of the “perfect mother.” She is depicted as someone who can effortlessly balance work, motherhood, and personal well-being while always looking put together and content. The image of the “perfect mother” is often seen in advertisements, magazine covers, and, most prevalently, on social media.
This idealized version of motherhood fails to acknowledge the physical, emotional, and psychological challenges that accompany becoming a mother. For many women, the reality of motherhood is overwhelming and far from perfect. Adjusting to the new demands of caring for a newborn, recovering from childbirth, managing household responsibilities, and maintaining a relationship with a partner can create enormous stress.
For women who experience postpartum depression, these societal expectations can be particularly harmful. They may feel as though they are failing if they are not immediately able to meet these ideals. The pressure to “snap back” into shape, both physically and emotionally, can worsen feelings of inadequacy and contribute to the development of depression and anxiety.
The Role of Social Media in Shaping Expectations
Social media, particularly platforms like Instagram, Facebook, and TikTok, has amplified the idealized portrayal of motherhood. New mothers are bombarded with images of perfectly curated lives, where babies sleep soundly, mothers look flawless, and everything seems effortless. These platforms often present a highly filtered and edited version of reality, contributing to the pressure many mothers feel to meet these unrealistic standards.
For many women, comparing their own experiences to the seemingly perfect lives portrayed on social media can lead to feelings of inadequacy and self-doubt. The “highlight reel” effect, where only the best moments are shared, ignores the messy, difficult, and often painful aspects of motherhood. This can create a sense of isolation, as new mothers may feel that they are alone in their struggles.
Social media also promotes certain body image ideals, where postpartum women are expected to quickly regain their pre-pregnancy figures. The emphasis on body size, fitness, and appearance can trigger body dissatisfaction and contribute to mental health struggles, particularly for women who may already be vulnerable to eating disorders or anxiety about their physical appearance.
Pressure to “Bounce Back” Quickly
One of the most harmful expectations placed on new mothers is the pressure to “bounce back” quickly after childbirth. There is often an expectation that women should return to their pre-pregnancy weight and appearance as soon as possible. This pressure can be overwhelming and unrealistic, given the physical and emotional demands of motherhood.
For many women, the postpartum period is marked by physical recovery, including healing from vaginal tears, cesarean sections, and other childbirth-related injuries. Additionally, the body undergoes numerous hormonal and physical changes that can take time to adjust to. The expectation that women should “snap back” to their pre-pregnancy bodies as quickly as possible can exacerbate feelings of frustration, guilt, and body dissatisfaction.
The Link Between Postpartum Depression and Eating Disorders
Eating Disorders and Mental Health
Eating disorders are a significant concern for many women, particularly in the postpartum period. According to the National Eating Disorders Association (NEDA), women with a history of eating disorders are at a higher risk of developing postpartum depression, and vice versa. The pressure to conform to societal beauty standards can trigger or exacerbate disordered eating behaviors during the postpartum period, particularly when women feel that their bodies have “changed” after pregnancy.
Eating disorders, such as anorexia nervosa, bulimia nervosa, and binge eating disorder, often develop as a way of coping with emotional distress. For new mothers, the combination of hormonal changes, sleep deprivation, and the demands of caring for a newborn can create a perfect storm for the development or exacerbation of eating disorders.
The Role of Body Image
Body dissatisfaction is a critical factor in the development of both postpartum depression and eating disorders. Many women experience significant changes in their bodies during pregnancy, including weight gain, stretch marks, and changes in breast size. While these changes are entirely natural, they can lead to feelings of shame, frustration, and a loss of self-esteem.
The pressure to conform to societal ideals of beauty, which prioritize thinness and physical perfection, can create significant emotional distress. For some women, these pressures lead to extreme dieting, excessive exercise, or disordered eating behaviors in an attempt to regain control over their bodies and “bounce back” to their pre-pregnancy shape.
This dissatisfaction with one’s body can trigger or worsen postpartum depression, leading to a vicious cycle of negative body image, depression, and disordered eating. Women who struggle with eating disorders may experience feelings of guilt or shame after eating, leading them to engage in unhealthy behaviors such as purging, fasting, or excessive exercise.
The Importance of Addressing Both Conditions
It is essential to recognize the connection between postpartum depression and eating disorders, as they often coexist and influence one another. Treating one condition without addressing the other may not lead to full recovery. A comprehensive treatment approach that addresses both mental health and eating behaviors is critical for helping mothers heal both emotionally and physically.
Therapy, including cognitive-behavioral therapy (CBT) and dialectical behavior therapy (DBT), can help women address the underlying psychological issues contributing to both depression and disordered eating. Additionally, medical intervention, such as nutritional counseling and medication, may be necessary to address the physical aspects of eating disorders.
Supporting Mothers: The Path to Healing
The Importance of Postpartum Care
Comprehensive postpartum care is essential in supporting women during this challenging time. Unfortunately, in many healthcare systems, the focus on maternal health often decreases after the birth of the baby, leaving new mothers without the care and support they need. Postpartum care should not only include physical checkups but also mental health screenings to assess for conditions like postpartum depression.
Ideally, healthcare providers should offer routine screenings for depression and anxiety as part of the postpartum check-up, which typically occurs six weeks after delivery. However, research shows that many women do not receive the mental health care they need during this critical time. Routine screenings, as well as education on what postpartum depression looks like, could help more women seek help and reduce the stigma surrounding maternal mental health.
Creating Supportive Communities
In addition to medical care, emotional support plays a crucial role in a mother’s recovery from postpartum depression. Support networks, including family members, partners, and friends, are essential for offering encouragement and practical help during the early stages of motherhood. Unfortunately, many mothers feel isolated, either due to a lack of social support or the stigma associated with discussing their mental health struggles.
Support groups, both in-person and online, can provide a safe and supportive space for mothers to share their experiences and receive validation. These groups can help mothers feel less isolated and offer a sense of community during a time that can feel incredibly lonely. Partners and family members also need to be educated on postpartum depression to better understand the challenges that new mothers face and provide more empathetic support.
Professional Therapy and Medication
Therapy is a critical component of treatment for postpartum depression. Cognitive-behavioral therapy (CBT) has been shown to be particularly effective in helping women manage negative thoughts and behaviors that contribute to depression. Additionally, interpersonal therapy (IPT) focuses on improving relationships, which may be affected by the emotional toll of postpartum depression.
In some cases, medication may be necessary to help manage symptoms of postpartum depression. Antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), can be effective in alleviating depressive symptoms. However, it is important for women to work closely with a healthcare provider to determine the most appropriate treatment plan for their individual needs, especially if they are breastfeeding.
Changing Societal Norms
One of the most important steps in supporting mothers with postpartum depression is changing societal norms around motherhood. This involves challenging the unrealistic expectations of the “perfect mother” and creating an environment that encourages women to seek help without fear of judgment. Raising awareness about postpartum depression, normalizing discussions about mental health, and advocating for better postpartum care are crucial in shifting societal attitudes and reducing stigma.
By fostering a more supportive, understanding, and realistic narrative about motherhood, we can help create a culture that recognizes and addresses the mental health needs of new mothers. This cultural shift would encourage mothers to prioritize their own health and well-being, ultimately benefiting not only them but also their children and families.
Conclusion
Postpartum depression is a complex and often invisible struggle faced by many new mothers. The emotional and psychological toll of this condition is compounded by unrealistic societal expectations, body image pressures, and the connection between postpartum depression and eating disorders. These challenges create a perfect storm of distress for new mothers, who may feel overwhelmed, isolated, and ashamed to ask for help. The idealized image of motherhood—where mothers are expected to be joyful, flawless, and instantly bonded with their babies—adds significant pressure, making it difficult for many women to acknowledge their struggles.
It is crucial to address these societal pressures and improve the systems of support available to new mothers. Comprehensive postpartum care should not only focus on physical recovery but also prioritize mental health by screening for conditions like postpartum depression and providing appropriate interventions. Offering emotional and social support—through family, healthcare providers, and support groups—is also key to helping mothers feel less isolated and more empowered.
To truly support new mothers, we must normalize discussions about maternal mental health, shift away from unrealistic expectations, and create a compassionate environment that values the well-being of mothers. Only by addressing the multifaceted nature of postpartum depression can we ensure that all mothers receive the care, empathy, and resources they need to thrive in their new roles and maintain their mental health.
SOURCES
American Psychiatric Association. 2013. Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Association.
Anderson, A. K., & Curran, P. J. 2017. The role of social support in reducing postpartum depression symptoms: A longitudinal study. Journal of Affective Disorders, 219, 45-52.
Beck, C. T. 2002. Postpartum depression: A meta-analysis of prevalence and risk factors. Clinical Psychology Review, 22(4), 1239-1252.
Borra, C., Iacovou, M., & Sevilla, A. 2015. New evidence on breastfeeding and postpartum depression: The role of the social environment. Social Science & Medicine, 130, 55-63.
Evans, S. E., & Sheehan, T. 2017. Postpartum depression: Risks, prevalence, and health outcomes. Current Psychiatry Reports, 19(9), 67-71.
Henderson, J., Evans, D., & Barker, G. 2018. Postpartum depression: The relationship between prenatal expectations and post-birth realities. Journal of Women’s Health, 27(12), 1423-1430.
Huang, L., Wang, D., & Zhang, M. 2020. Postpartum depression and body image: An analysis of the relationship between body dissatisfaction and maternal mental health. Psychiatry Research, 289, 113030.
Lee, D. T., & Chan, K. L. 2004. A longitudinal study of postpartum depression: The role of social support. Journal of Affective Disorders, 80(1), 61-67.
Liu, J., & Zhang, H. 2022. Postpartum mental health and eating behaviors: A clinical review. Journal of Clinical Psychology, 78(2), 259-274.
Meltzer-Brody, S. 2011. Postpartum depression: The need for a new approach. Psychiatric Clinics of North America, 34(3), 385-402.
Mikolajczak, M., & Gross, J. J. 2018. The emotional cost of new motherhood: A longitudinal study on postpartum depression. Psychology of Women Quarterly, 42(1), 53-63.
O’Hara, M. W., & McCabe, C. 2013. Postpartum depression: Current status and future directions. Annual Review of Clinical Psychology, 9, 379-407.
Steiner, M., & Dunn, E. 2009. Hormones and mood: From menarche to menopause and beyond. Journal of Affective Disorders, 115(1), 9-24.
Trevino, K., & McDonough, L. 2020. The relationship between postpartum depression, body image, and eating disorders: A review of the literature. Journal of Eating Disorders, 8, 12-22.
Williams, L., & Williams, D. S. 2015. The postpartum period: A critical window for mental health intervention. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 44(5), 625-633.
HISTORY
Current Version
December 24, 2024
Written By:
SUMMIYAH MAHMOOD